Access to healthcare is often among the most difficult battlegrounds for transgender people, especially those who wish to undergo medical transition. Though the DSM’s continued inclusion of “gender dysphoria” is deeply problematic in that it serves to pathologize trans existence, it regretfully does have some benefits within the broken state of the U.S.’s present medical insurance and healthcare industries. Most simply, it gives trans people a fighting chance to receive coverage for gender-affirming care.
Most insurance companies actually require that an individual receive a diagnosis of gender dysphoria before receiving coverage for treatments related to their transition, including hormone replacement therapy, top surgery, bottom surgery, facial feminization surgery, and more.
Unfortunately, this diagnosis is subject to heavy gatekeeping within the mental health industry, and access to trans-affirming professionals can be prohibitively expensive and difficult to locate. For transgender folks who are unable to access affirming care, the looming specter of needing to “prove” that they are transgender in order to get that little “F64.9” DSM code in their patient chart is often enough to deter them from pursuing treatment at all.
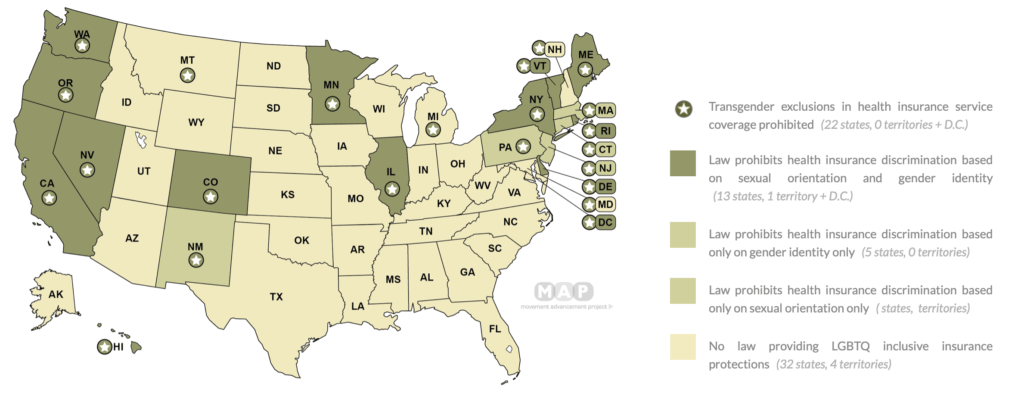
Even for trans folks who are able to receive this diagnosis, it can still be incredibly difficult to receive coverage for gender affirming care. To start, coverage varies greatly by state and by provider. In 29 U.S. states, insurance law still grants providers the right to flat out refuse coverage for transition-related healthcare.
Furthermore, there are a number of procedures for which insurance companies deny coverage nearly across the board because they consider these to be “cosmetic.”
Although transgender folx have repeatedly asserted that procedures like facial hair electrolysis, pre-bottom surgery genital electrolysis (which reduces the extremely uncomfortable possibility that hair grows inside the vagina after vaginoplasty, and many surgeons require you to complete prior to bottom surgery), and nipple reconstruction after a masculinizing top surgery are medically necessary and alleviate gender dysphoria, many insurance companies continue to refuse medical coverage by asserting that “cosmetic procedures are not medically necessary.”
(Here is a comprehensive list of insurance companies that will consider coverage for hair removal in conjunction with a diagnosis of gender dysphoria)
I began to pursue my medical transition.
As I mentally prepared to come out as transgender publicly, the first transitional step I felt prepared to take was scheduling laser treatments to reduce my facial hair growth. Nothing causes me quite the degree of dysphoria as the appearance and feel of my face as those tiny black specks make their brutal appearance across my chin, and I was extremely excited at the prospect of getting rid of them once and for all.
To me, the idea of transitioning felt much more feasible if I didn’t have to worry about growing a beard on top of everything else I’d have to navigate. At that time, my primary goal in transitioning was to be read as cisgender, and I worried that 5 o’clock shadow would make it significantly harder to “pass” (to use a common yet problematic term).
As I researched my insurance company’s policies on gender transition, I was incredibly disheartened to learn that even with a diagnosis of Gender Dysphoria, my insurance company was unwilling to cover the cost of hair removal because they considered the procedure “cosmetic.” I found myself dealing with the prospect of dishing out a whopping $1,350.00 for a mere five sessions, which I absolutely could not afford to pay out-of-pocket on my $10/hour barista wages.
As I continued to research coverage, I was further saddened to realize that this stance was uniform across the insurance industry. I spent several months feeling incredibly defeated, and nearly gave up on pursuing laser treatments altogether until my wonderful mother suggested we sell my old saxophone, which had been hiding in the closet for years (much like my teenage self…)
A local shop bought my sax for $1,000.00, leaving $350.00 that I ultimately decided to pay out-of-pocket. Since most people need at least ten if not closer to fifteen sessions to reduce hair growth to a comfortable minimum, I suspected I would eventually have to budget almost $4,000.00 if I continued to undergo this medically necessary treatment. I ended up only being able to afford those five, and continued to deal with crippling gender dysphoria as my facial hair continued to grow, which often interfered with my ability to engage socially or go about my daily activities.
To this day, [Starbucks] remains among a very small group of U.S.-based employers that offer coverage for gender-affirming procedures that many insurance providers consider “cosmetic.”
Starbucks pioneered their Supplemental Health Insurance Plan for trans healthcare.
Two years later, Starbucks pioneered a transender-inclusive health insurance policy which promised to cover any transition-related care performed in a medical facility that was not covered under an employee’s main insurance plan. Starbucks’ Supplemental Plan was positively revolutionary. To this day, the company remains among a very small group of U.S.-based employers that offer coverage for gender-affirming procedures that many insurance providers consider “cosmetic.” In order to access coverage under this plan, Starbucks Partners need only be enrolled in company health insurance and receive an admittedly elusive diagnosis of gender dysphoria.
While this plan has been life-changing for many Partners — myself included — and has covered nearly $1500 worth of my laser treatments, it has one unfortunate limitation — it only covers procedures performed in a medically-certified treatment center. As Starbucks negotiated coverage for procedures that insurance companies had formerly declined to include, they refused to back down from this stipulation.
Initially, the impact of this requirement on my ability to access reimbursement was minimal — it simply meant that I had to go to a specific laser provider in Manhattan. However, many folks outside of big cities have found that the closest certified facility is several hours away, which creates an extreme barrier to care — an experience that is sadly all too familiar for many transgender people.
Note: If you are a Starbucks Partner looking to access the supplemental plan, call 1-866-849-7103.
As I began to prepare for bottom surgery, I learned that I would have to undergo anywhere from 15-75 hours of genital electrolysis in order to mediate the risk of intra-vaginal hair growth following my operation. Even though many surgeons require that transgender folx undergo this procedure prior to vaginoplasty, and many insurance companies agree that bottom surgery is medically necessary for many transgender people, the vast majority of insurance companies still consider genital electrolysis to be cosmetic. Therefore, transgender people hoping to undergo bottom surgery often find themselves responsible for thousands of dollars in fees for genital hair removal on top of a mountain of other transition-related costs.
Note: For more information about your employer, insurance provider, and general questions about transgender healthcare, read HRC’s Transgender-Inclusive Healthcare Coverage and the Corporate Equality Index.
I was denied coverage for genital electrolysis.
Because I work for Starbucks, I felt blessed as I prepared to enter this phase of my journey because I assumed that my electrolysis would be covered. I reached out to Starbucks Advocacy, Starbucks’ Liaison between Partners and the supplemental plan provider, to ask for a list of electrolysis providers in my area that were covered under their plan.
Days later, I received a call back — “no providers available.” None! I was baffled. In New York City, a veritable hub of transgender healthcare, they could not find a single electrolysis provider that fit their criteria for reimbursement. Furthermore, my insurance provider has not yet joined the list of providers that offer coverage for genital electrolysis, so I could not turn to my provider for funds. With up to $11,000.00 on the line, I quickly panicked as I tried to understand this apparent discrepancy.
This is just one of the countless ways that the healthcare industry is failing the transgender community, even under the most seemingly trans-affirming of medical plans.
I inquired further about why I had been able to access laser hair removal but not electrolysis. My advocate explained that laser hair removal is frequently performed in facilities that also perform cosmetic surgeries, which means that many of these facilities employ licensed surgeons. The same cannot be said for most facilities that offer electrolysis, which leaves most if not all electrolysis treatments ineligible for reimbursement. Unfortunately, because genital hair removal must be completely permanent and laser treatments are not, it is crucial that transgender folx use electrolysis for this purpose.
This is just one of the countless ways that the healthcare industry is failing the transgender community, even under the most seemingly trans-affirming of medical plans. Several trans masculine folks in my life have lamented that when receiving their bill for top surgery, they were horrified to realize that although the physical removal of breast tissue was covered, they were charged exorbitant fees for nipple reconstruction. How, exactly, insurance companies maintain that nipple reconstruction is cosmetic after acknowledging that top surgery is necessary to treat gender dysphoria is truly beyond comprehension.
Among trans feminine folx, access to coverage for procedures like Facial Feminization Surgery (FFS) and Breast Augmentation (BA) is extremely limited. While many transgender women notice significant feminization in our chests and facial appearance after a few years on HRT, many others do not. For a number of trans feminine folks, these surgeries are the only way to adequately alleviate our gender dysphoria. However, many transgender women are denied coverage on the grounds that they do not meet their insurance company’s incredibly arbitrary criteria for these procedures to be deemed medically necessary.
For many trans and gender non-conforming folx, gender-affirming care is medically necessary to alleviate gender dysphoria.
Let me be perfectly clear — the current literature on gender dysphoria is not on the side of exclusionary policies. The WPATH Standards of Care, which set the precedent for evidence-based, affirming medical and mental health treatment of transgender people, assert that procedures or treatments that feminize or masculinize the body are often medically necessary to alleviate gender dysphoria. However, insurance companies remain reluctant to adapt in order to adequately support transgender health, often asserting that doing so would be cost-prohibitive. This is a pattern with insurance companies — justifying their decision to belligerently ignore the medical necessity of certain treatments in order to cut costs, further marginalizing entire communities in the process.
As long as insurance companies withhold the right to deny us coverage, the onus is on employers to negotiate for more inclusive coverage on behalf of their transgender employees. It is crucial that companies take this responsibility seriously. Among other trans-affirming policies, one major precursor to creating a truly accessible workplace for trans and gender non-conforming people is to offer comprehensive, gender-affirming benefits.
Contrary to a common assertion, offering this care is not cost-prohibitive for insurance providers nor employers, but it is cost-prohibitive for the vast majority of transgender people to pay out of pocket. Since our ability to access affirming, transgender-competent care is inextricably tied to our mental and physical well-being and therefore our ability to be mentally and physically present for 40+ hours a week in our place of work, trans competent care is a workplace issue. Transgender people are not set up for success in the workplace until employers enact a gender-affirming benefits package that is available to all employees.
Employers — especially large employers — it is time to step up your game.
Go to bat with insurance companies and demand trans-inclusive healthcare. Make clear to these companies that you will no longer pay into their plans if they decline to offer comprehensive coverage for gender-affirming care. Once you’ve developed a fully accessible, comprehensive benefits package for transgender employees, distribute this information company-wide. While I do happen to love working for Starbucks, a precursor to true equity for TGNC folx is that our access to comprehensive healthcare is not limited by where we choose to work. We have the right to seek employment wherever we want without fear that we will be denied coverage for medically necessary treatment. This is non-negotiable.
The cost of transgender healthcare is just one among many barriers to care for trans folx. Currently, 29 states lack discrimination protections for transgender people who use private healthcare, meaning that private insurance companies in these states withhold the right to deny coverage for any transition-related services. Even when procedures are covered, practitioners tend to be severely lacking in trans-competency, due largely to the extreme rarity of LGBTQ+-specific training courses for medical and mental health professionals.
Furthermore, a 2019 Trumpian attack on the transgender community called the “Conscience Rule” proposed to give practitioners the right to refuse treatment to LGBTQ+ patients by citing moral or religious beliefs. LGBTQ+ advocates were troubled by the policy’s ambiguous language, which paved the way for doctors to claim religious exemptions from providing life-saving care to LGBTQ+ folks. Though this ruling was eventually struck down in federal court, it set an extremely dangerous precedent within the healthcare industry by asserting a doctor’s right to refuse to help a person in need.
Putting pressure on employers to include comprehensive benefits for transgender people is a great start to establishing trans-inclusive healthcare as the norm, but it is certainly not the whole fight. I will continue to explore issues in healthcare accessibility on this blog and I would love to hear your thoughts.
What are some questions you have about transgender healthcare? If you are TGNC, what are some problems you have had in access to healthcare?
Send your thoughts by submitting the form below!




This article was really helpful – I learned so much. It’s wonderful that large employers like Starbucks are paving the way, but more can definitely be done.
thank you so much for reading! I’m really glad you found it helpful!
The sad reality between FtM and MtF is for many of us, we (FtM) often just need HRT, a mastectomy, and a hysterectomy for the majority of dysphoric relief, and we can obtain that without trans-specific language. A good therapist can be vague with insurance to get the mental health visits covered. A knowledgeable gynecologist can get the right tests “authorized” to dictate the need for surgery, as gynecological health cannot be denied. For HRT, well any pharmacy discount card can knock off a good amount of the price that of comes within usual copay range (me here in Jersey is like $11/vial, when the pharmacy charges $27/vial full price, for generic testosterone cyponiate). I hope for any of your readers who are AFAB and identify somewhere on the masculine-of-center side of things, I hope this information helps. ✌️
Thank you so much for your thoughts! You added a lot of valuable info here!
Pingback: Six TGNC Folx Share How Visibility Paves the Way to a Transer Future • Trans & Caffeinated
Pingback: SPOTLIGHT ON Em Rabelais • Trans & Caffeinated
Pingback: 6 inspiring TGNC Folx Share How Visibility Paves the Way to a Transer Future • Trans & Caffeinated
Pingback: Trans Existence and This Crazy Little Thing Called "Passing" • Trans & Caffeinated
Pingback: Spotlight On Em Rabeleis: Transgender in the Early Era of SARS-COV-2 • Trans & Caffeinated
Pingback: Healthcare is a Basic Human Right. Here are 9 Ways You Can Support the Trans Community Today. • Trans & Caffeinated